Communication Between Medical Practitioners and Dancers
Ruanne Lai, Donna Krasnow, M.S., and Martin Thomas, Ph.D.
Journal of Dance Education • Volume 12, Number 2, 2008.
Abstract
The purpose of this study was to investigate patterns of communication between professional and pre-professional dancers and medical practitioners. One survey was developed and randomly conducted among family physicians, sports medicine physicians, chiropractors, physical therapists, and registered massage therapists. A second survey involved volunteer ballet and modern dancers in professional dance training programs, college and university dance programs, and independent dance artists. One hundred and ninety questionnaires were distributed to medical practitioners, and 50 were returned. Of 380 questionnaires given to dancers, 202 were returned. The dancers were 18 to 49 years old, with a majority between the ages of 18 and 20. They averaged more than 10 years of dance training. All of the questionnaires were distributed in a single large Canadian city.
The data shows that medical practitioners rarely communicated with each other concerning a common (dance) patient. They also failed to communicate, in most cases, with the dancers’ teachers, choreographers, and directors. This was not disconcerting to injured dancers, who tended to believe that such communication was not important to their recovery. Significantly, dancers did not fully understand the nature of their injuries when they sought medical advice, and they did not press the medical practitioners for additional information. Both groups generally believed that dancers would benefit by learning more about human anatomy.
Studies indicate that annual musculoskeletal injury rates in professional dance companies and pre-professional dancers range from 67% to 95%. [1-6] The occurrence and recurrence of injuries are related to the type of dance being practiced, and the dancers’ technique, experience, physiology, and even psychological factors. [7-10]
Injuries may be accompanied by pain, the medical symptom that most often motivates people to seek medical care, [11] but the perception of pain is not a valid indicator of the severity of injury. Furthermore, the perception of pain varies widely among dancers, even for identical injuries, and perceived severity of pain is negatively correlated with the levels of both skill and experience. [12-13]
Injured dancers often fail to seek medical attention, [14-15] due in part to concern for losing time from training or performing. They are inclined to self-diagnose and self-treat, as they do not feel understood by medical practitioners, who are perceived as being unaware of the vocabulary and physical demands of dance [14,16] and lacking dance-specific psychological training. [17] In some cases the costs of medical care or ongoing treatment and follow-up are prohibitive. [14,18] When a dancer does seek medical care, successful treatment may not result for various reasons, including: a lack of caregiver training in dance-related injuries, a failure of the dancer to understand clearly the nature of the injury, and the dancer’s noncompliance with the recommended treatment. [19,20]
The objective of this study was to investigate the perceptions of dancers and professional medical practitioners (PMPs) with regard to their communication concerning the treatment of dance-related injuries, specifically:
1. Their respective perceptions about communication between PMPs and dancers;
2. Their respective perceptions about communication between PMPs and dance teachers and choreographers;
3. Their respective perceptions about communication between/among medical practitioners concerning dancers’ injuries;
4. Their respective perceptions about PMPs’ explanations of injury assessments;
5. Dancers’ self-reported understanding of treatment protocols discussed; and
6. Dancers’ self-reported compliance with treatment protocols.
Methods
The study received approval by the appropriate ethics review committee at the researchers’ university. All subjects provided written confirmation of their informed consent.
Participants: Medical Practitioners
The target sample of PMPs was obtained by randomly selecting from the phonebook 28 names of each of the following types of providers: family physicians, sports medicine physicians, chiropractors physical therapists and registered massage therapists. A 50-item questionnaire was mailed to these 140 practitioners. Follow-up was conducted by telephone. In addition, 50 questionnaires were selectively distributed by hand to sports medicine clinics that were known to treat a large number of dancers. In these clinics, PMPs were asked to return the completed consent forms and questionnaires by mail.
The questionnaire consisted of three parts. Part A included demographic questions such as type of practice, sex, and age. Part B asked about their professional practice and involvement in dance: years of practice, percentage of patients who are dancers, activities related to dance, attendance at conferences or seminars related to sports medicine, attendance at conferences related to dance medicine, familiarity with current sports medicine and dance medicine literature, time allotted for assessment, and the importance of their dancer-patients’ understanding human anatomy. Part C dealt with the PMPs’ perceptions and attitudes pertaining to communication with dancers about treatment and recovery. In Part C, response sets for most questions were 10-point interval scales, with verbal definitions of only the two extreme values.
Participants: Dancers
The questionnaire distributed to dancers differed from the questionnaire given to health-care providers, but addressed the same issues. In many cases the items on the two questionnaires were identical or directly comparable. The dancers’ questionnaire also consisted of 50 items. Again, most response sets were 10-point intervallevel scales.
The sample of dancers was a convenience sample. Questionnaires were distributed to 308 dancers in a university dance program, and 72 were distributed at an emerging-dance-artists’ conference for graduating dance students in professional dance training programs, postsecondary institutions, and independent dance artists. In addition, three questionnaires were emailed to participants over the age of 18 in a pre-professional training program.
The questionnaire for dancers also consisted of three parts. Part A included questions on the dancer’s age, sex, and dance activities. Part B asked about training, such as years, type, occurrence of injuries during dance training or outside of dance practice, type of health-care providers or other caregivers from whom dancers sought advice when injured, and time between onset of injury and subsequent visit to a practitioner. (Injury was defined subjectively by the participants. Recurrence of an injury was defined as a continuation of the previous injury of that type.) In Part C, dancers were asked questions that corresponded to Part C of the PMP questionnaire.
Results
Medical Practitioners
In the random sample, the return rate was 17.5% (N = 35); in the selectivelychosen sample, where sports clinics treated more dancers, the return rate was 30.0% (N = 15). Two of the 50 respondents did not treat dancers and were excluded from the analysis. Of the remaining 48, 30 were female. Not all professions were equally represented; 36.0% (N = 18) were physical therapists, 34.0% (N = 17) chiropractors, 16.0% (N = 8) registered massage therapists, and only 10.0% (N = 5) sports medicine physicians. An additional 4% identified themselves as athletic therapists.
A large number of respondents (44%) were in the 30-39 age cohort. Years of practice varied widely: 28% had practiced for 1 to 4 years, 24% for 5 to 10 years and 24% for 11 to 15 years. Most PMPs (86%) indicated that fewer than 20% of their patients were dancers, and, as noted previously, two respondents had no dancers as patients.
Although 70% of respondents had participated in various forms of dance, and 32% had some dance training, 20% had never even observed dance.
All but one of the PMPs had attended at least one sports medicine conference or seminar, and 54% had attended such conferences more than ten times, but only 22% had ever attended a conference or seminar related to dance medicine. Similarly, although the majority of respondents (58%) read the sports medicine literature frequently, only 32% have ever read dance medicine literature. The PMPs’ infrequent attendance at dance science conferences, and failure to regularly read dance medicine literature, may partly explain Smith’s findings that dancers often do not feel understood by doctors. [16]
Despite the overall lack of familiarity with dance medicine, half of the PMPs considered it “essential” for dancers to understand basic human anatomy, and 24% thought it “moderately important.” One respondent considered it “detrimental” for dancers to understand anatomy.
The following discussion concerns PMPs’ interactions with injured dance patients. Because two respondents did not have any dance patients, the data are based on a sample of 48.
Respondents stated that it typically took 15 to 30 minutes to assess an injured dancer. The PMPs years in practice correlated with their perceptions of both the amount of time they spent assessing technical habits (r = .29, p < .05) and the perceived amount of improvement in their dance patients after treatment (r = .34, p < .05). Higher perceived improvement rates also were reported by those practitioners who asked dancers about technique (r = .45, p < .01).
PMPs who saw dance relatively frequently tended to report more communication with dance teachers (r = .30, p < .05), with artistic directors (r = .30, p < .05), and with other medical practitioners (r = .44, p = < .01). The practitioner’s level of dance training was positively correlated with the level of communication with other involved practitioners (r = .34, p < .05), but unrelated to communication with dancers’ teachers and artistic directors.
The number of dance patients in a practice was positively correlated with the reported frequency of reading dance literature (r = .323, p < .05) and attendance at dance medicine conferences or seminars (r = .46, p < .01). The number of years in practice was also positively correlated with reported attendance at these conferences or seminars (r = .34, p < .05). Practitioners who read the dance medicine literature most frequently were also likely to report communication with other practitioners treating the same dancer (r = .30, p < .05), as well as a greater inclination to inquire about technical habits (r = .35, p < .05) and a greater likelihood of assessing those habits (r = .38, p < .01).
Practitioners’ communication with dance teachers was positively correlated with their perception of dancers’ understanding of the treatment protocol (r = .33, p < .05). Practitioners’ perception of dancer’s willingness to alter harmful dance technique habits was positively correlated with level of communication with choreographers (r = .42, p < .01) and with artistic directors (r = .32, p < .05). The level of PMP communication with other practitioners was positively correlated with perceived patient improvement (r = .31, p < .05). The variable most strongly correlated with perceived patient improvement, however, was perceived patient compliance with prescribed treatment (r = .46 p < .01).
Dancers
Of 380 questionnaires distributed, 202 (53.2%) were returned. Of these respondents 53.0% were 18 to 20 years old, and 39.1% were 21 to 24 years old. They averaged more than ten years of dance training. Undergraduate students represented 65.8%, professional dance school students 32.7%, dance teachers 15.8%, and professional dancers 4.5% of the respondents. Females comprised 92.1% of the sample. Most dancers had training in more than one form of dance: 197 in ballet, 196 mentioned modern dance, 155 cited jazz, 105 in musical theater, 45 in flamenco and Spanish, 44 in tap, and 43 in hip-hop. More than half (50.5%) of the dancers had training in ballet or modern plus at least one other form, such as flamenco or Spanish, Irish or Scottish, African Caribbean, Chinese, or Indian.
Of the dancers, 68% believed that it was essential to their dance training to understand basic human anatomy (compared to 50% of the medical practitioners), and none thought it “unnecessary” or “detrimental.”
Throughout the course of their training, 13.5% had been injured once during practice, 45.5% had been injured 2 or 3 times, and 7.0% had been injured more than 10 times.
Outside of dance practice, 67.8% of the dancers had been injured 1 to 3 times, and 3.0% had been injured more than 10 times. After an injury, only 32% of dancers visited a medical practitioner within 3 days.
On a scale where “1” represented perceived “significant deterioration” and “10” represented perceived “significant improvement,” dancers were asked to rate the outcomes of advice or information given by the various kinds of practitioners. In this regard, 142 dancers reported on the advice from family physicians, 106 dancers rated sports medicine physicians, and 128 dancers commented on physical therapists; these were the most frequently rated professions. The mean score for the perceived quality of advice from family physicians was 4.43 (SD = 2.34), for sports medicine physicians 7.03 (SD = 2.23), and for physical therapists 7.62 (SD = 2.23). Results from analysis of variance indicate that type of practitioner consulted had a significant effect on dancers’ perception of deterioration or improvement (p < .001).
Dancers were asked to indicate, on a 10-point interval scale, the extent to which they would be willing to affect or alter certain kinds of behaviors. Overwhelmingly, they reported a high willingness to learn basic human anatomy (M = 9.16, SD = 1.53), to follow prescribed treatment protocols (M = 8.94, SD = 1.13), and to alter dance technique habits during a rehabilitation period (M = 8.47, SD = 1.70). However, dancers were less willing to alter technique habits in the long term (M = 7.09, SD = 2.38). Willingness to alter technique habits was found to be significantly higher in the short term than in the long term (p < .001). Finally, dancers’ willingness to decrease frequency of training activities (M = 6.64, SD = 2.33) was significantly lower (p < .001) than their willingness to decrease intensity (M = 7.43, SD = 2.03), t = 6.67. In summary, injured dancers were willing to modify dance practice only temporarily, and they often resisted reducing hours of dance training.
Finally, on a 10-point scale measuring “importance” (where “1” represented “of little importance”), dancers were asked to rate various issues related to their PMP’s practice. To a dancer, the PMP’s communication with either the dancer’s teacher (M = 5.67, SD = 3.10) or choreographer (M = 5.11, SD = 3.08) was only moderately important. Of much greater concern was communication between the PMP and other medical practitioners treating the same injury (M = 7.32, SD = 2.89). Other aspects of PMP behavior important to injured dancers were the number of years in practice (M = 7.13, SD = 2.43), the percentage of clients who were dancers (M = 7.34, SD = 2.45), attendance at dance medicine conferences (M = 7.41, SD = 2.51) or sports medicine conferences (M = 7.84, SD = 2.15), and regular reading of dance medicine literature (M = 7.49, SD = 2.39) or sports medicine literature (M = 7.85, SD = 2.17).
The amount of time allotted for assessment was considered important (M = 7.53, SD = 2.33). The single variable of greatest importance to dancers was the frequency with which practitioners observed dance (M = 8.15, SD = 2.21).
Communication among Medical Practitioners, Dance Teachers and Choreographers
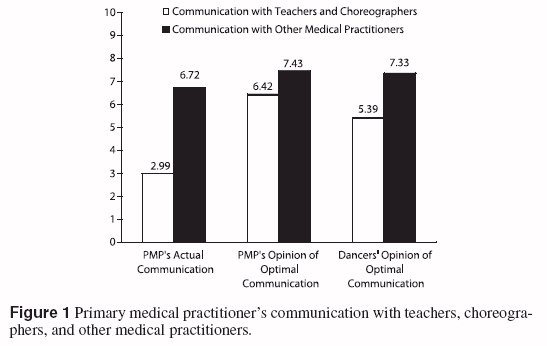
Dancers’ and PMPs’ responses were almost identical concerning the importance of practitioners’ communication with other relevant healthcare providers (7.33 and 7.43, respectively). They also had similar views about the importance of PMP communication with teachers and choreographers (5.39 and 6.42, respectively). Figure 1 compares the primary medical practitioners’ reporting of actual communication with their view of optimal communication; it also describes dancers’ views of PMPs’ optimal communication. The left bar in each case represents practitioners self-reported communication with teachers and choreographers, and the right bar represents self-reported communication with other medical practitioners.
Inquiry and Assessment of Technical Habits and Pre- and Post-Injury Activity
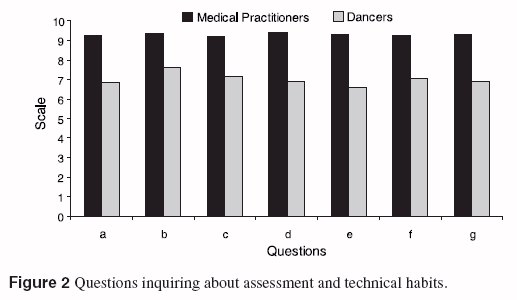
Both medical practitioners and dancers were asked if the practitioner generally inquired about the following issues: 1. when did the dancer intend to resume activity; 2. how frequently did the dancer participate in activity prior to the injury; 3. how intense was activity prior to the injury; 4. how frequent would activity be after recovery; 5. how intense would activity be after injury recovery; 6. how frequent was participation during the recovery period; and 7. how intense was participation during the recovery period . Figure 2 compares the respective perceptions of dancers and PMPs about the frequency with which each of these injury-related questions is asked. There is a consistent difference in perception. For each of these issues concerning a dancer’s activity before and after the injury, practitioners are more likely to report having asked the question than dancers are to recall having heard it.
Table 1 describes these data for each question for each group, and tests of significance concerning mean differences in dancers’ and health practitioners’ reports. The difference between what the practitioners claim they ask and what the dancers believe is asked is significant with regard to each of the seven pairs of questions (p < .001).
Discussion
Medical practitioners and dancers had similar views with respect to the importance of practitioner’s communication with other healthcare providers, and with dance teachers and choreographers. The small differences suggest that PMPs ascribed greater importance to both of these kinds of communication than did dancers. We find it interesting that both groups did not attach even more importance to communication between primary healthcare providers and secondary providers. Given the manifest importance of this kind of communication, we had expected responses to reflect that. A second interesting aspect of these data is the seeming discrepancy between what practitioners say about the importance of communication with other healthcare providers and the frequency with which they attempt that kind of communication. One could infer from this discrepancy that some practitioners were attempting to give “right answers” instead of honest ones, or perhaps they considered such behavior important as they indicated but still less important than some other factors that were not measured, such as their (uncompensated) time. Practitioners claimed they frequently inquire about dancers’ physical practice prior to and after an injury, but dancers recalled that their PMPs often failed to ask these kinds of questions.
It had been expected that dancers would be more willing to comply with treatment protocols if they better understood the nature of their injuries and the treatment process. However, this was not found to be the case. This lack of compliance is likely the result of financial, psychological, social, or aesthetic concerns that overshadow health issues. [21-24] Most of these concerns collectively stem from the culture of dance. The dancer’s body is part of the dancer’s identity, [22,25] and in ballet injuries are perceived to be an inevitable part of the vocation. [10,26] Although the majority of dancers who participated in the current study were not professional ballet dancers, all of them had ballet training. Wainwright has argued that “Dancer’s attitudes to pain are embodied, and they epitomize the connections between the individual (dancer) and the (ballet) institution. Being a dancer requires a stoic attitude to pain—indeed, injury, pain and suffering were seen as playing a central role in the development of artistic sensitivity.” [10] Of course, the notion of working through pain and suffering is not exclusive to dance; similar attitudes are found throughout amateur and professional sports. [27-29]
Previous research indicates that among injured collegiate dancers the common depressive symptoms of increased fatigue and loss of energy were ameliorated after dancers received physical therapy. [23] Yet many dancers, perhaps because they fear social isolation, ignore the first symptoms of injury. [24] Further, our data suggest that many resist following treatment protocols over the long term if they perceive that such compliance would interfere with their training or performance.
Compliance with treatment protocols is also affected by the desire to achieve an aesthetic ideal. Body dissatisfaction and the desire to lose weight are greater in ballet students than non-physically active students. [24] When dancers are told to rest because further activity would delay their recovery they may choose not to comply, ironically, because of the desire to remain fit and retain skill levels. The fear of losing control over one’s body may explain our finding that injured dancers are more compliant with respect to decreased intensity of dance training than with respect to decreased frequency.
Moreover, many injured young dancers do not seek advice from teachers on improving their technique to avoid future injury. [30] Fear of peer disapproval may partly explain why dancers, and especially young ones, are reluctant to make long-term changes in technique; such changes could be seen as a rejection of the commonly accepted (or endured) practices of their peers.
In addition to the issues of concern to student dancers, professional dancers may encounter financial problems. If dance is a vocation, taking time off for treatment may mean both loss of income and additional medical expenses. Based on the complex issues facing injured dancers, it is recommended that in conjunction with prescribed physical treatment dancers receive explicit information on the probable consequences of compliance and noncompliance. This may appear to be nothing more than patient informed consent, but informed consent is often understood to mean understanding the probable consequences of a prescribed treatment. In a population in which noncompliance is problematic, as with dancers, informed consent should be understood to include an explicit description of the probable consequences of noncompliance.
The majority of dancers and medical practitioners believed that it was “essential” for dancers to understand basic human anatomy, and dancers reported a high willingness to do so. This finding may provide an impetus for dance programs and dance studios to incorporate dance science education as part of a holistic approach to dance training. If this kind of information is not offered, dancers may increasingly self-educate about anatomy and dance kinesiology.
One limitation of this study is that the dancers and PMPs are not directly linked. That is, the practitioners surveyed do not correspond perfectly with the PMPs that the dancers refer to, and the dancers who participated in the survey are not necessarily those described by the practitioners. Any comparison of the responses of these two groups must reflect this fact. (Because the survey was done in a single city, and because all but one of the health care providers who responded has seen patients who are dancers, it is likely that some are linked, which somewhat ameliorates the problem. However, no attempt was made to link individual dancers to individual healthcare providers.)
This problem is compounded by the fact that the proportion of practitioner respondents representing each type of practice does not correspond to the proportions seen by the dancers after an injury. The most extreme example is that no family physicians returned questionnaires, whereas a family physician is the type of medical practitioner most often seen initially by young dancers after an injury.
This lack of comparability does not prevent us from comparing expressions about what is important in PMP-dancer interactions, but they are relevant if we try to compare recollections of treatment patterns. Both sets of recollections of events may be entirely accurate, even though they are different. For example, when the stated recollections of our dancer respondents do not appear consistent with the recollections of healthcare providers with regard to time spent in assessment, that discrepancy may be due in part to the fact that physical therapists, sports medicine specialists, chiropractors, and massage therapists tend to spend more time in assessment than do family physicians.
Of course, data based on recollections may also be invalid for a number of reasons common to survey research: the respondents may give answers that are self-serving, or their recollections may be imperfect.
Conclusion
In the past decade interest in dance medicine and science has increased significantly, as evidenced by the growing number of academic journals and conferences devoted to the topic. Organizations such as the International Association for Dance Medicine & Science, the Performing Arts Medicine Association, and the Performing Arts Special Interest Group of the Orthopedic Section of the American Physical Therapy Association strive to educate healthcare professionals, dance educators, and dancers. They support research and promote best practices in performing arts medicine. Unfortunately, many healthcare professionals who treat this unique class of patients have little or no dance-specific knowledge and skills; a significant number have never seen theatrical dance in performance. Even when such knowledge and skills are applied, their utility will be limited if communication between healthcare providers and their dancer patients is ineffective. Similarly, the effectiveness of treatment will certainly be compromised if dancers fail to understand clearly the effects of noncompliance with treatment protocols, as well as the ways in which social, aesthetic, and psychological factors tend to reduce compliance.
About the Authors
Ruanne Lai, is a masters of science dandidate in the Graduate Programme in Kinesiology and Health Science at York University, Toronto, Ontario, Canada.
Donna Krasnow, M.S., is in the Department of Dance at York University, Toronto, Ontario, Canada. Martin Thomas, Ph.D., is in the Department of Political Science, and School of Public Policy and Administration, at York University, Toronto, Ontario, Canada.
References
1. Anderson BD. Cost containment of a professional ballet company through in-house physical therapy. J Orthop Sports Phys Ther. 1999;29:A19.
2. Bronner S, Ojofeitimi S, Rose D. Injuries in a modern dance company: effect of comprehensive management on injury incidence and time loss. Am J Sports Med. 2003;31(3):365- 73.
3. Kerr G, Krasnow D, Mainwaring L. The nature of dance injuries. Med Probl Perform Art. 1992;7(1):25-9.
4. Nilsson C, Leanderson J, Wykman A, Strender LE. The injury panorama in a Swedish professional ballet company. Knee Surg Sports Traumatol Arthrosc. 2001;9(4):242-6.
5. Solomon R, Solomon J, Micheli LJ, McGray E Jr. The “cost” of injuries in a professional ballet company: a five-year study. Med Probl Perform Art. 1999;14(4):164-9.
6. Byhring S, Bø K. Musculoskeletal injuries in the Norwegian National Ballet: a prospective cohort study. Scand J Med Sci Sports. 2002;12(6):365- 70.
7. Barrell GM, Terry PC. Trait anxiety and coping strategies among ballet dancers. Med Probl Perform Art. 2003;18(2):59-64.
8. Patterson EL, Smith RE, Everett JJ, Ptacek JT. Psychosocial factors as predictors of ballet injuries: interactive effects of life stress and social support. J Sport Behav. 1998;21(1):101-12.
9. Poczwardowski A, Conroy DE. Coping responses to failure and success among elite athletes and performing artists. J Appl Sport Psychol. 2002;14(4):313-29.
10. Wainwright SP, Williams C, Turner BS. Fractured identities: injury and the balletic body. Health. 2005;9(1):49-66.
11. Cordell WH, Keene KK, Giles BK, et al. High prevalence of pain in emergency medical care. Am J Emerg Med. 2002;20(3):165-9.
12. Paparizos AL, Tripp DA, Sullivan MJL, Rubenstein ML. Catastrophizing and pain perception in recreational ballet dancers. J Sport Behav. 2005;28(1):35-50.
13. Encarnacion MLG, Meyers MC, Ryan ND, Pease DG. Pain coping style ballet performers. J Sport Behav. 2000;23(1):20-32.
14. Krasnow D, Kerr G, Mainwaring L. Psychology of dealing with the injured dancer. Med Probl Perform Art. 1994;9(1):7-9.
15. Mainwaring L, Kerr G, Krasnow D. Psychological correlates of dance injuries. Med Probl Perform Art. 1993;8(1):3-6.
16. Smith TJ. Injury management in professional dance companies (M.A. thesis, Brigham Young University). (Microform Publications: University of Oregon No. UO 98 429—UO 98 430), 1997.
17. Gordon S, Milios D, Grove JR. Psychological aspects of the recovery process from sport injury: the perspective of sport physiotherapists. Aust J Sci Med Sport. 1991;23(2):53- 60.
18. Garrick JG, Requa RK. Ballet injuries: an analysis of epidemiology and financial outcome. Am J Sports Med. 1993;21(4):586-90.
19. Scialom M, Gonçalves A, Padovani CR. Work and injuries in dancers: survey of a professional company in Brazil. Med Probl Perform Art. 2006;21(1):29-33.
20. Macchi R, Crossman J. After the fall: reflections of injured classical ballet dancers. J Sport Behav. 1996;19(3):221-34.
21. Krasnow D, Mainwaring L, Kerr G. Injury, stress, and perfectionism in young dancers and gymnasts. J Dance Med Sci. 1999;3(2):51-8.
22. Mainwaring L, Krasnow D, Young L. A teacher’s guide to helping young dancers coping with psychological aspects of hip injuries. Journal of Dance Education. 2003;3(2):57- 64.
23. Sanahuja-Maymo, M, Pérez-Testor C, Virgili C. Depressive symptoms and associated factors in a sample of injured collegiate dancers. In: Proceedings of the 16th Annual Meeting of the International Association for Dance Medicine & Science, 2006, pp. 264-268.
24. Ravaldi C, Vannacci A, Bolognesi E, et al. Gender role, eating disorder symptoms, and body image concern in ballet dancers. J Psychosom Res. 2006;61(4):529-35.
25. Mainwaring L, Krasnow D, Kerr G. And the dance goes on: psychological impact of injury. J Dance Med Sci. 2001;5(4):105-15.
26. Barnes MA, Krasnow D, Tupling SJ, Thomas M. Knee rotation in classical dancers during the grand plié. Med Probl Perform Art. 2000;15(4):140- 7.
27. Lavallee D, Robinson HK. In pursuit of an identity: a qualitative exploration of retirement from women’s artistic gymnastics. Psychol Sport Exerc. 2007;8(1):119-41.
28. Malcom NL. “Shaking it off” and “toughing it out”: socialization to pain and injury in girls’ softball. J Contemp Ethnogr. 2006;35(5):495- 525.
29. Roderick M. Adding insult to injury: workplace injury in English professional football. Sociol Health Illness. 2006;28(1):76-97.
30. Robson BE. Am I going to be good enough for this profession? Emotional reactions to injury in ballet students. In: Proceedings of the 16th Annual Meeting of the International Association for Dance Medicine & Science, 2006, pp. 19-23.